UCD - Urea Cycle Disorders Education & Support
Urea cycle disorders (UCDs) are a group of inherited, genetic disorders. The urea cycle is a chain of reactions using a group of enzymes in the liver. These enzymes are important in removing unneeded protein byproducts (nitrogen) from the blood. Excess nitrogen can come from the diet when more protein is eaten than the body can use. Nitrogen can also come from breakdown of protein in muscles and other body stores. Normally, excess nitrogen enters the urea cycle to produce urea, a nontoxic compound that is eventually excreted in urine. When one of the enzymes in the urea cycle is not working, urea cannot be produced. Instead, the excess nitrogen ends up as ammonia.
Ammonia (abbreviated NH3) is a toxic compound. When it builds up in the blood, high amounts can cause many health problems, mainly in the nervous system. Symptoms of high ammonia levels in infants and young children can include severe weakness (lethargy), abnormal breathing, seizures and eventually coma if not treated aggressively. Long term problems can include poor growth, slow development and learning problems.
| The names of the urea cycle disorders are based on the enzyme that is affected: | |
| NAGS deficiency | N-acetylglutamate synthetase deficiency |
| CPS 1 deficiency | Carbamylphosphate synthetase 1 deficiency |
| OTC deficiency | Ornithine transcarbamylase deficiency |
| ASS deficiency or Citrullinemia | Argininosuccinate synthetase deficiency |
| ASL deficiency or Argininosuccinic Acidura | Argininosuccinate lyase deficiency |
| ARG 1 deficiency or Argininemia | Arginase 1 deficiency |
Incidence, Genetics and Newborn Screening
UCDs occur in about 1 in every 10,000 births. The most common UCD is OTC deficiency. Urea cycle disorders can occur in all ethnic groups.
Most UCDs are inherited as “recessive disorders.” In recessive disorders, both the mother and father are “carriers,” and they do not have any symptoms of the disorder. With each pregnancy there is a 1 in 4 (25%) chance that the infant will be affected. OTC deficiency is an "X-linked disorder," meaning the abnormal gene is located on the X chromosome. This usually means boys have more severe symptoms than girls, but this can vary. A genetic counselor can help explain the inheritance of the disorder and the risks to future infants.
Some of the UCDs can be screened for at birth through a simple blood test. For details on newborn screening (NBS) in the US, visit https://newbornscreening.hrsa.gov/your-state; for information on NBS in Canada, visit https://www.raredisorders.ca/.
The primary nutritional management for UCDs is a low protein diet. Special medical formulas and low protein foods are often part of the diet. With the low protein diet, high protein foods are often avoided or strictly limited, as too much high protein food can lead to high ammonia levels. These include milk and dairy products, meat, poultry, fish, eggs, beans, nuts and peanut butter. Regular breads and pastas may be allowed, but low protein versions of these foods are often used in the diet. Vegetables and fruit are allowed. Foods may be weighed or measured to ensure that excess protein is not consumed. Special low protein foods allow for more choices in the diet and less concern that the person will eat too much protein.
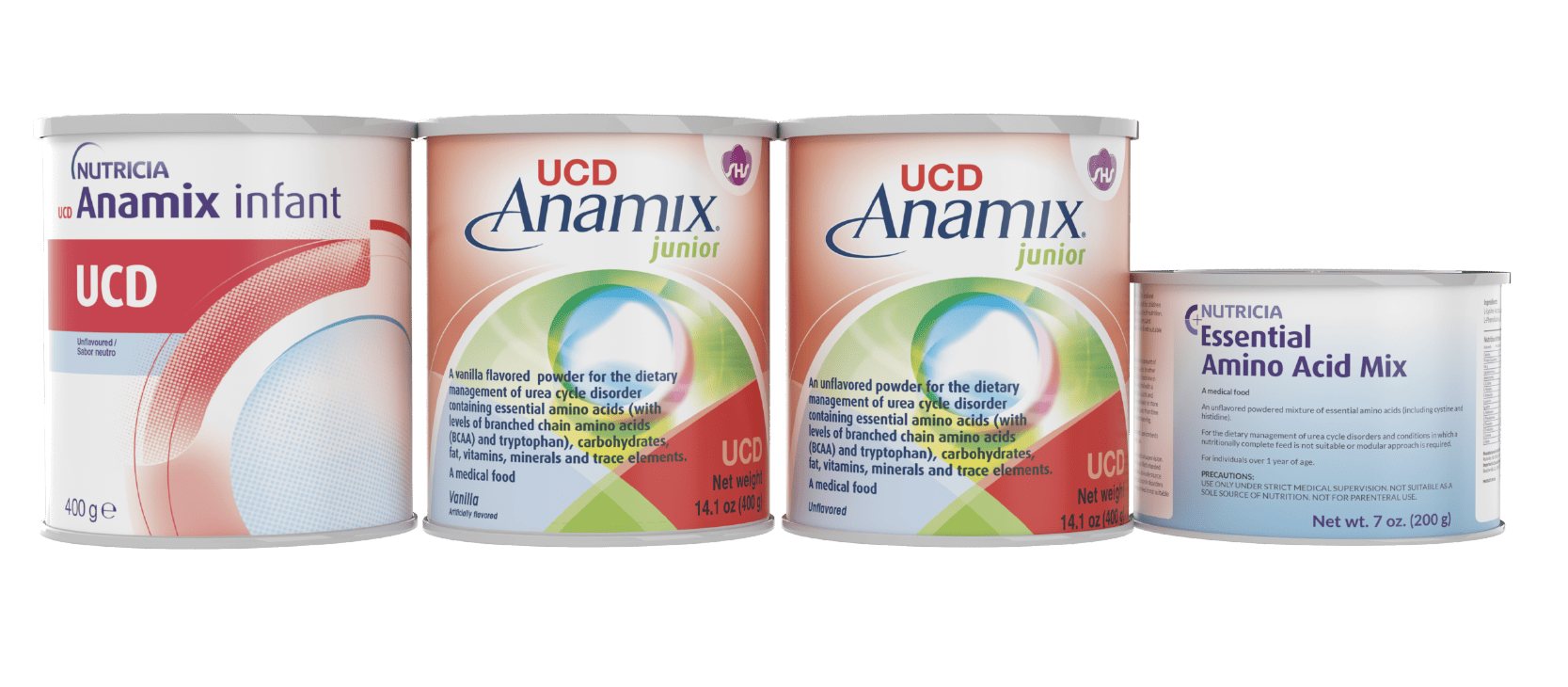
Often, a special UCD medical formula is also part of the diet for people with a urea cycle disorder. Medical formulas provide calories from carbohydrate and fat plus vitamins and minerals, but do not have excessive protein. In UCD medical formulas, the source of protein is “essential amino acids.” These amino acids are called “essential” because the human body cannot make them, and we must get them from the diet. Amino acids, including essential ones, are used by the body for growth and development. Adding a UCD medical formula to a child’s diet can make it easier to give just enough protein for growth, but not an excessive amount that produces too much nitrogen. A metabolic dietitian will work closely with people with a UCD to prescribe the best diet plan and help with needed changes in the future.
Nutricia North America provides a range of medical formulas as well as low protein foods. Please contact us for more information. Your dietitian will help you decide which products are best.
There are also some drugs designed to help manage UCDs. A metabolic physician may prescribe these to help prevent high ammonia levels. Because these drugs can cause a decrease in the blood levels of three essential amino acids (leucine, valine and isoleucine), UCD medical formulas from Nutricia have more of these amino acids to help prevent deficiency. In some instances it might be necessary to supplement with one or more of these specific amino acids. Another medical option for some patients with a UCD is a liver transplant. Your metabolic physician will discuss the options that are best.
During Illness
During an illness or after an injury, the body increases the breakdown of protein from muscles and organs. This increases the risk of high ammonia levels, which can lead to serious medical problems. Early signs of high ammonia levels can include vomiting, excessive sleepiness, coordination problems and/or changes in mental status. During any illness, it is very important to notify your metabolic clinic right away. Often, the diet is adjusted to decrease or remove protein and increase calories. This can help slow the breakdown of protein from the body. Medications may also be adjusted during illness. Your clinic will give you an emergency letter – if you notice signs of high ammonia levels, take this letter to the emergency room. During serious illness, a hospital stay may be needed.
Nutricia North America would like to thank Sandy van Calcar, PhD, RD, Oregon Health & Science University for her consultation.
Low Pro Living Support
We have a library of information to help support families like yours throughout the various stages of life's journey. From big moments, like starting college to little ones like what to eat for dinner, we have tips and ideas to help you along the way.